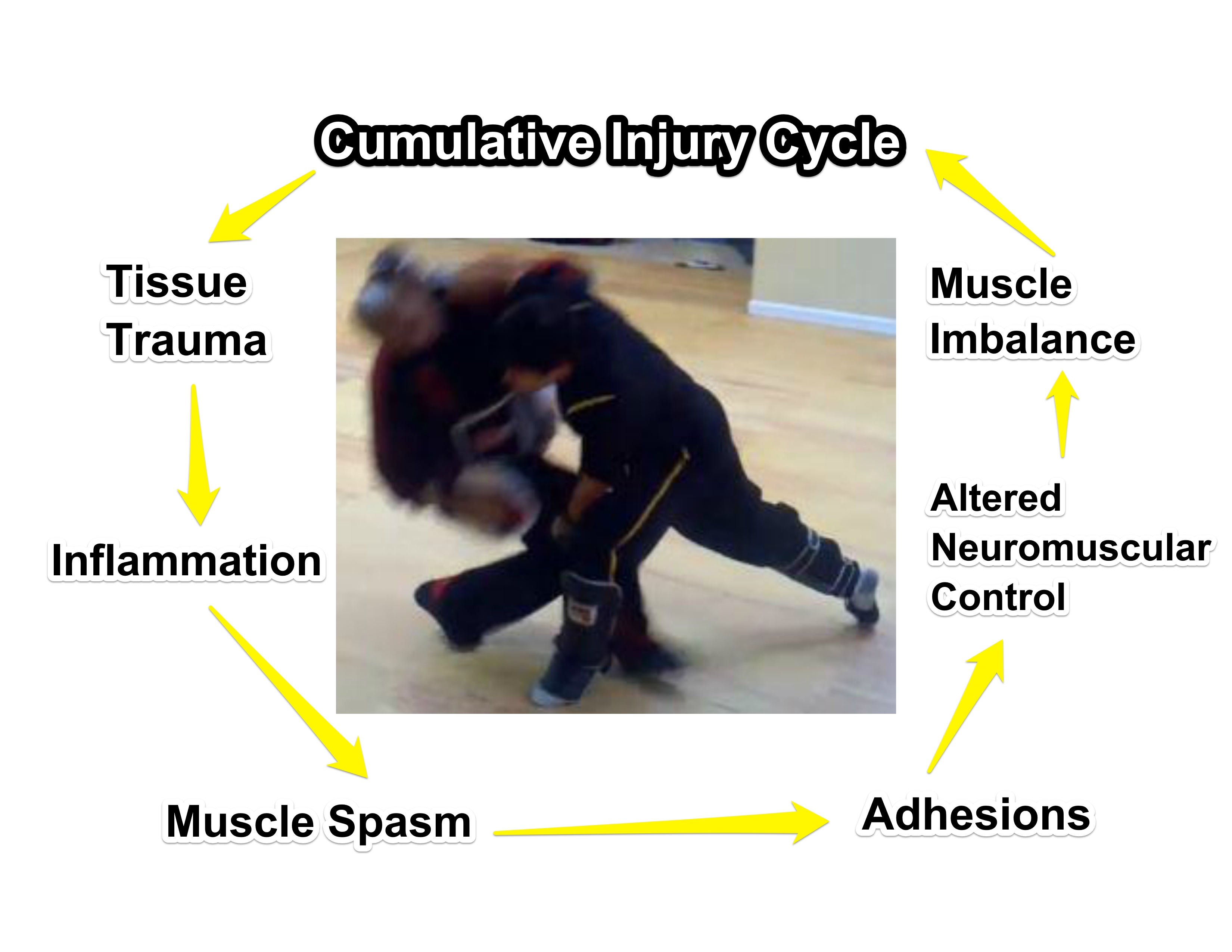
Pain free does not equal restorative function. Neglected injuries induce altered neuromuscular control, which in turn retard skill development.Photo: Author
The point is, training injuries are common and can set you back. Taking a break from training or training without regard to your injury both jeopardize your personal defense preparedness. You should continue learning, but special attention to movement patterns is required when you train while protecting and rehabilitating the injury.
The solution? Accelerate your rate of recovery with proactive injury management.
Hypothesis
Whether you are injured in training or any other way, you should take responsibility to work toward recovering rather than strictly leaving healing in the hands of medical professionals. No one knows your physical habits better than you do, and there will be no medical professional to helicopter parent your injury throughout the day. The goal of this article is to provide you with fundamental information about mechanisms of injury and recovery, so that physical therapists, chiropractors, or any other medical professionals support your recovery rather than limit your recovery to symptom reduction.
Although there’s a wide spectrum of injuries ranging from contusions, bruises, and abrasions to more severe conditions including calcification of muscles and brain swelling, the scope of this article is narrowed to injuries associated with mobility outside of bone fractures. You have the most control and accountability for your physical habits and lifestyle, which in turn gives you the most opportunity to speed recovery with your personal effort and cognizance.
Soft-Tissue Injuries
Sprains, strains, aches, and pains. We’ve all experienced these to some degree. To better understand how and why the boo boo hurts, let’s first take a look at some basic anatomy associated with common injuries.
Types of Tissue
Fascia: Fascia or myofascia tissue is dense connective tissue that surrounds all of your muscles and bones and gets plenty of blood flow. The study of myofascia is a relatively new field of research that has discovered breakthroughs in explaining how trigger point therapy, acupressure, and acupuncture work. Myofascial injuries are a result of repetitive strain that has produced what we know as “knots” in our muscles, which trigger a muscle imbalance cascade.
Muscle: Muscle is what facilitates movement, and is a product of a synergistic agonist and antagonist design. Motion is achieved through a process of reciprocal inhibition, which means that when your bicep flexes, the opposing muscle, the tricep, relaxes relative to the bending motion. Overuse injuries program one muscle to be hyperactive and tight, while the opposing muscle becomes lazy and out of shape. This can further result in bad posture, bad coordination, and tendonitis.
Post-workout recovery should also be noted as an injury, because many people emphasize protein. But without proper glycogen replenishment, a carbohydrate that is the muscles’ preferred energy source, cellular adaptation (muscle size) and neuro adaptation (strength) may be compromised. Nourishment and rest are the keys to regeneration. Improper nourishment and insufficient rest lead to overtraining injuries. Both overuse injuries and overtraining result in muscle strain related injuries.

Tendon injuries present greater opportunity for proactive injury management. *Coccyx face not actual medical disorder.* Photo: Author
Ligaments: Ligaments receive the least amount of blood flow. They simply connect bone to bone with dense flexible collagen for joint stabilization, and only facilitate movement by way of tissue pliability. Unlike fascia, tendons, and muscles, which can be lengthened and shortened with activity, ligaments can only be lengthened when stretched beyond their normal range of motion. Ligament sprains and associated capsules are the most difficult to remedy due to the reduced amount of blood flow and their irrelevance to motion.
Symptom-Free Is Not Malfunction-Free
More often than not, we take measures to block the brain from knowing that our weapon systems are malfunctioning, so we continue operating with less efficient gear. The whole “Motrin and water” joke is just that. Not only do Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) not fix you, they worsen you by inhibiting the immune system while simultaneously giving you the false sense of returned mobility and range of motion, which is likely to exacerbate the injury. Relative to the immediate need for mobility such as in the context of the Military, it can make sense that NSAIDs such as Motrin, Ibuprofen, and Naproxen are applied. But for most other circumstances, NSAIDs are not a good solution. To better understand why, let’s take a look at how the body heals.
Stages of Injury and Healing
1. Reaction: Acute Inflammatory Phase
24 to 72 hours of injury. The immune system triggers an inflammatory response often characterized by pain, swelling, and increased local temperature. These are good things. The pain tells you to stop moving, and the swelling and increased temperature are the immune system doing its thing. Blood clots seal the damage, myofilament reactions are triggered, and phagocytosis flushes out the edema and cell debris.
Inflammation becomes dysfunctional when swelling is excessive, which is often the case with trauma to high blood flow tissues like the belly of the bicep muscle. The inflammation pathway is paved by lipids known as prostaglandin. The biosynthesis of prostaglandins is blocked by NSAIDs, which is how the injury becomes asymptomatic, or without pain. If the pain is unmanageable, NSAIDs can help in no other way than by blocking the pain signal. By blocking the prostaglandin production, you also block the body’s healing cascade.
2. Regeneration: Sub-acute Fibro-elastic/Collagen Repair Phase
48 hours up to six weeks. Fibroblasts synthesize scar tissue, commonly known as scabs. The collagen lays down the building blocks for new tissue, while capillary budding occurs to improve tissue nourishment by bringing nutritious blood to the area.
3. Remodeling
Three weeks to one year. The maturity of collagen results in a shrinking tight scar, manifested as a knot. The functional capabilities of the muscle and tendon are improved by the remodeling of collagen. But the process of fibrosis inhibits restorative muscle regeneration. Imagine having a scab on your skin. The scab shrinks, and the local area of the skin loses its pliability and breathability. Fibrosis competes with muscle repair by inhibiting the lengthening, shortening, and blood flow at the collagen site.
4. Cumulative Injury Cycle: Chronic Phase
Ongoing until injury cycle is addressed. Neglected knots at the injury site result in adhesions that alter coordination, or specifically, neuromuscular control. The compensated movement patterns overwork other muscles while underutilizing the injured site. The resulting fatigue in weakness creates a muscle imbalance, which causes strains and sprains and triggers the inflammatory response.

Ligament injuries are difficult to manage due to limited ability to tighten stretched soft tissue such as the ACL or MCI. *Coccyx face may not always present at time of injury.* Photo: Author
Fixing and Priming Your Gear
A physical therapist can pinpoint the mechanism of injury and identify which muscles need to be tightened and which need to become more pliable. How you go about proactive injury management will be relative to the severity of the injury. The recommendations listed here are fundamental concepts that can help accelerate healing as a supplement to the instructions provided by your medical professional.
1. Reaction Phase
Immobilize the injury site and allow the immune system to operate. Water intake and nutrient-dense antioxidant food consumption are the best actions you can take during this phase. If the pain interferes with your ability to function in your daily life, NSAIDs can be taken and ice can be applied to dull the pain. If the pain is tolerable, it is better to avoid the two, as NSAIDs inhibit the healing process, and ice slows immune activity at the injury site.
2. Regeneration Phase
Begin testing range of motion. Massage peripheral muscles that may have seized near the injury site. Apply heat to the injury site to increase blood flow and improve pliability of collagen.
3. Remodeling Phase
This phase is critical to restore functional capabilities while avoiding muscle imbalances and the resultant cumulative injury cycle. Here is the process of proactive injury management:
a. Massage adhesions: As previously mentioned, fibrosis can inhibit the healing process and trigger a cascade that leads to the cumulative injury cycle. Identifying where the adhesions, or knots, are located is best done by a deep tissue massage therapist. However, the knotted areas are recognizable by their tenderness when pressed. Self Myofascial Release techniques can be applied via foam rollers, golf balls, and frozen water bottles.
It is best to break up the adhesions with a cold muscle as opposed to warmed up. This is because warming up makes the peripheral tissue pliable, which then becomes similar to trying to roll dough on a trampoline. Massaging the cold muscle is much more efficient at breaking up the scab that surrounds the injury site.
b. Strengthen: Soft-tissue injuries are often associated with lengthened tissue that is generally opposite the areas where the knots are found. Strengthening the weak muscles prevents muscle imbalances and teaches newly generated tissue how to move and thus restores normal neuromuscular control.
Strengthening is a two-part process of activating specific muscles in isolation, followed by integrating the targeted muscles to contextual movement. Generally, three sets of 20 with a one-minute break between sets is recommended.
c. Stretch: The most efficient stretch is known as Proprioceptive Neuromuscular Facilitation. PNF stretches exploit the concept of reciprocal inhibition. By contracting the quadriceps during a toe touch, a signal is sent to the hamstrings to deactivate, resulting in increased range of motion.
PNF stretching is done by reaching a stretch threshold, contracting the opposing muscle for 30 seconds, and then pushing through the range of motion. Following an isolated PNF stretch, it is recommended to perform dynamic stretching in contextual motion. An example of a dynamic stretch for tight hip flexors is a lunge with trunk rotation. A dynamic stretch in context is a lunge with high compressed ready/weapon retention rotation.
d. Deep Heat: Ultrasound, moxa, rubber water bottle, or Jacuzzi time contributes to the improved blood flow from the previous activity. Deep heat targets the adhesions to further soften them and improve the phagocytosis process of removing dead tissue while supplying fresh, nourishing blood to the newly constructed site.
The proactive injury management process should prevent the cumulative injury cycle, and is also the process of breaking out of the cumulative injury cycle caused by old, neglected injuries.
Conclusion
Well, that was a lot of serious face to explain a way to stay proactive with training while managing your injury intelligently. There are many antiquated methods that I didn’t address for the sake of relative brevity, but I’m hoping that by looking at how the body’s healing process works, you can deduce how and why certain treatment modalities may be less efficient. Of course, none of this would have been necessary if Mr. Dunning-Kruger McTriestoohard wasn’t such a coccyx.
Share tips, start a discussion or ask one of our experts or other students a question.
Already a member? Sign in

I sincerely wish that I knew even one quarter of what you're talking about but I can't even follow along the written word
This was the best explanation of I juries and recovery that I've ever read! Thanks!
Certified Athletic Trainers are a very effective but under used resource for injury management. They specialize in active people and utilize training in injury management.
Love to learn
Thank you for an excellent article and for covering a critical topic for all martial artists and those interested in self defense. There's an old saying, "Injuring yourself is doing your enemies work."
Great information and well explained. Thanks a lot
I've had two herniated lumbar disks for years. I've heard that strengthening abs holds the lumbar spine in alignment, because the back muscles are not strong enough. Please write another tutorial about spinal injuries/chronic pain/muscle spasms that malign the spine.
Good article. The science is not settled on the topic of the use of NSAIDs in the context of healing and recovering from injury. We do know that they provide pain relief, and can reduce inflammation. But the potential negative effects that the author points out are confounded when people overuse medications or use them to enhance performance. The age old advice still holds true: Know thyself. Each individual body can be a little different in how healing and recovery proceeds, and each can have different responses to the use of medications like NSAIDs. Speaking for myself, I find them useful relieve various sore spots at the end of the day, but I never take them in order push myself further. And before you chuck your Advil into the trash, remember that there are also risks in using alternatives like acetaminophen and aspirin. As always, let's not throw out the baby with the bathwater...
Thanks, there's a lot of good info here that I've never heard. What about RICE, then? Every doctor, therapist, you name it, any medical professional I've seen for injuries over the years has always said RICE is their recommended treatment plan.